More Information
Submitted: April 10, 2021 | Approved: April 27, 2021 | Published: April 29, 2021
How to cite this article: Raja A, Saifuddin PK, Shekhar N, Mann H, Sarma P, et al. Pre-eminence and comparative analysis of skin and surface disinfectants: A systematic review to pave the way for SARS-CoV-2 prevention. Int J Clin Virol. 2021; 5: 047-053.
DOI: 10.29328/journal.ijcv.1001035
Copyright License: © 2021 Raja A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: SARS-CoV-2; Quick body sanitation; Povidine iodine based soaps/surgical scrub; Tunnel system; Hand sanitizers and surface sanitizers
Pre-eminence and comparative analysis of skin and surface disinfectants: A systematic review to pave the way for SARS-CoV-2 prevention
Anupam Raja1, Saifuddin PK2, Nishant Shekhar3, Harvinder Singh4, Phulen Sarma5, Ajay Prakash6 and Bikash Medhi7*
1PhD Scholar, Department of Pharmacology, PGIMER, Chandigarh, India
2M.Sc student, Department of Pharmacology, PGIMER, Chandigarh, India
3RF, Ddepartment of Pharmacology, PGIMER, Chandigarh, India
4PhD Scholar, Department of Pharmacology, PGIMER, Chandigarh, India
5Young Scientist, Department of Pharmacology, PGIMER, Chandigarh, India
6Assistant Professor, Department of Pharmacology, PGIMER, Chandigarh, India
7Professor, Department of Pharmacology, PGIMER, Chandigarh, India
*Address for Correspondence: Dr. Bikash Medhi, Professor, Department of Pharmacology, PGIMER, Chandigarh, India, Tel: 9815409652; Email: [email protected]
More than 200 countries have been devastated by the SARS-CoV-2 pandemic. The health workers exposed to SARS patients have been confirmed to be infected with coronavirus (SARS-CoV-2), regardless of the degree of their exposure. The increasing complexity of virus existence and heterogeneity has cast doubt on disinfectants as a viable choice. Hence, the present systematic review aims to achieve the comparative analysis of established disinfectants against enveloped and non-enveloped viruses including SARS-CoV and MERS-CoV. Three databases (Pubmed, Google scholar, and Medline) were searched to frame the systematic review. Our comparative analyses with 34 studies have found that 85% ethanol-based hand sanitizers and 7.5% Povidine Iodine based soaps/surgical scrub could be used to deter the SARS-CoV-2 virus as preferred hand sanitizers. For surface eradication, 0.5% sodium hypochlorite or a mixture of glutaraldehyde, Quaternary Ammonium Compounds (QAC), and isopropanol could have more efficacies as compared to hydrogen peroxide, phenol, and QAC alone. Moreover, the accelerated hydrogen peroxide as an active ingredient in the automatic quick surface disinfectant (tunnel system), maybe a positive indication for quick whole-body sanitation. Additionally, the alternative method for avoiding the rapidly increasing chain of infection with SARS and restarting regular life has been exclusively discussed.
The elementary structural composition of viruses consists of a genetic material (DNA or RNA), which might further vary as single-stranded or double-stranded. The second crucial component is the protective protein shell called the capsid, which guards the nuclear material against lytic degradation. This cluster of two components is called a virion. An auxiliary layer of the lipid membrane, derived from host cell membranes can be found on certain viruses which provide yet other consortia for the structural proteins that oblige to virus’s pathogenicity such as Spike and membrane glycoproteins [1]. The evolution of envelope glycoproteins has proven to increase the degree of infection severity, by mediating the cell-host membrane attachment and fusion for deadly viruses such as HIV-1, Gp2 Ebola, Influenza virus and Coronaviruses (SARS-CoV-1&2) [2]. The increasing structural complexity and variability of the virus have always challenged the choice of disinfecting agents. The troubling element about the viruses is that the closely related viruses show diverse susceptibility to the same class of disinfectants [3-6]. However, the frequently used chemical agents have shown a high affinity for the lipid-coated viruses compare to non-enveloped viruses, owing to their lipophilicity [4]. A great deal of dynamic equilibrium reaction goes into the dissolution of the viral structure upon the disinfectant treatment, which often causes an abrupt reversible multiplicity reactivation clumping of viral components that might retain the ability to infect in the disintegrated state [6]. Hence, an ideal preparation of an anti-virucidal agent should be based on a manifold of consideration from different scientific domains. Over 200 nations were affected by the severe acute respiratory syndrome (SARS-CoV-2) pandemic. It has been estimated that healthcare staff exposed to SARS patients may be contaminated with SARS coronavirus (SARS-CoV-2), irrespective of the exposure level [7]. A case-control study emphasized that wearing a face mask is the most effective method for preventing infections, followed by proper hand hygiene and surface sanitation [8]. Hands may be contaminated by patient secretions or contact with contaminated surfaces. SARS-CoV-2 has been reported to persist on surfaces for up to 96 hrs. In another prediction, dried SARS-CoV-2 sustained its viral load for six days, suggesting an exceptionally strong ability to survive. Only after nine days in a dry state does SARS-CoV-2 lose its infectivity [9].
The present systematic review is hypothesized to compare and analyze among the existing disinfectant action against enveloped and non-enveloped viruses including SARS-CoV, MERS-CoV, MHV (a potential surrogate for SARS-CoV) and canine coronavirus (CCV). The exclusive emphasis is on the efficiency of hand sanitizer’s action and which is as follows: Alcohol, Iodine + Povidine, Chlorohexidine, Soaps and Povidine iodine-based soap/surgical scrub; and surface disinfectant: Hydrogen peroxide, Phenol, sodium hypochlorite, and Quaternary Ammonium Compounds. Further, there have been disscussion of alternative methods which might help in stopping further spread of infection with SARS-CoV-2.
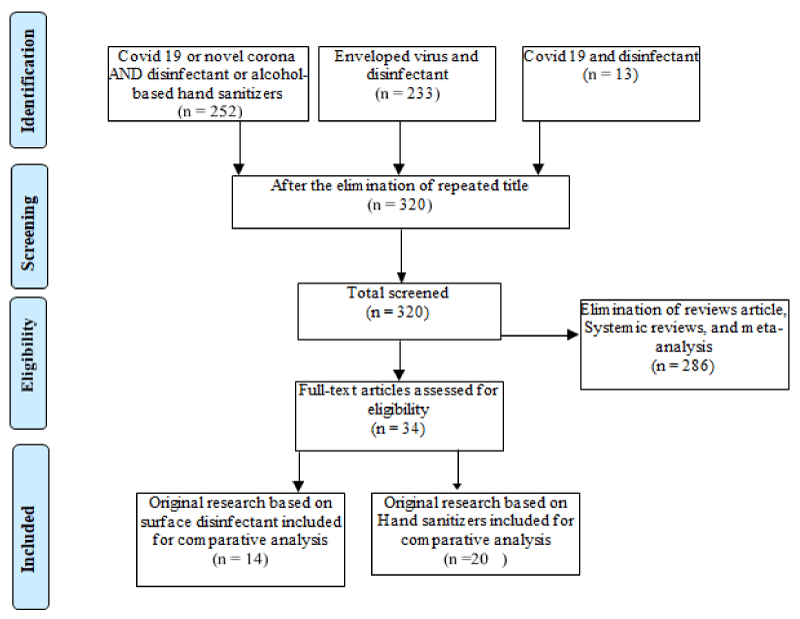
PubMed, Medline, and Google scholar databases were searched till August 27, 2020, for relevent studies. The following keywords were used, COVID-19 or novel corona AND disinfectant or alcohol-based hand sanitizers; enveloped virus and disinfectant and COVID-19 and disinfectant. Article extraction and duplicate removal was done using EndNoteTM X8.1 and MS-Excel. Details are given in PRISMA chart (Figure 1).
Figure 1: PRISMA chart showing the selection of studies for systematic review.
Enveloped virucidal and non-enveloped viruses based research article was mainly preferred for inclusion criteria and analysis purposes. Although, Reviews, systemic reviews, and meta-analysis were screened precisely for relevant material but not preferred for comparisons.
Routinely used hand sanitizers
Ethanol: Alcohol-based hand sanitizers (ABHS) are shown to have high efficacy in terms of virucidal activity. It may be used alone or in combination with other virucidal agents. Several studies have been performed to evaluate the efficacy of the gradient concentration of alcohol against viruses [10]. It has been reported that 80% of ethanol is effective against most of the enveloped and non-enveloped viruses [10], even the same concentration of alcohol is recommended by WHO for local production of alcohol-based disinfectant during infectious disease outbreak. Moreover, another study has been exclusively performed for SARS- CoV with three gradients percentage of ethanol (80%, 85%, and 95%), which reported 85% ethanol had a similar reduction, with no significant difference in reduction factor (log10) between 85% ethanol and 95% ethanol [11]. In contrast to this report, a combination of ethanol with other virucidal agents is shown to increase the potency of the ethanol even at a lower concentration. Three independent studies demonstrated different combinations ABHS. To make a convenient comparison, enumerations are assigned as Combinations 1, 2, and 3 (Tables 1,2).
| Table 1: Experimental evaluation of the antimicrobial activity of commonly used Hand sanitizers | ||||
| Ingredient | Percentage (%) | Time Duration(S) | Mean Log10 Reduction | Active Against (Studied Organism) |
| Ethanol (Rabenau HF et al. 2005) | 95 | 30 | 5.5 | SARS-CoV |
| Ethanol (Rabenau HF et al. 2005) | 85 | 30 | 5.5 | SARS-CoV |
| Ethanol (Steinmann J et al. 2013) | 80 | 30 | 5.38 | Adeno & norovirus SARS-CoV |
| Ethanol+ CHX (Biermann NM et al. 2019) | 61+1 | 30 | 3.1 | Bacteria |
| Ethanol+ CHX (Deshpande A et al. 2018) | 61+1 | 30 | 2.17 | Aerobic bacteria |
| CHX (Biermann NM et al. 2019) | 4 | 30 | 2.8 | Bacteria |
| Ethanol + 2-propanol+ Citric acid+Urea (Ionidis G et al. 2016 | 69.39 + 3.69 + 2 + 2 | 15 | 4 | Poliovirus, Murine norovirus (Enveloped viruses) |
| Ethanol+ Povidine Iodine (Eggers M et al. 2018) | 78+3.2 | 15 | 5.67 | Murine norovirus (Enveloped viruses) |
| Soap-potassium oleate (C18:1), sodium laureth sulfate (LES) and sodium lauryl sulfate (SDS) (Kawahara T et al. 2020) | - | 4 | Influenza virus | |
| Povidine iodine-based soap/surgical scrub (Eggers M et al. 2015) |
7.5 1 |
15 60 |
5.67 3.9-4.5 |
Ebola virus, Modified vaccinia virus Ankara (Enveloped) SARS-CoV |
| Table 2: Experimental evaluation virucidal activity of the commonly used surface disinfectant. | ||||
| Ingredient | Percentage (%) | Time Duration | Mean Log10 Reduction | Active Against(Studied Organism) |
| Hydrogen peroxide ( Sattar SA et al.1998) Accelerated Hydrogen peroxide (Omidbakhsh N et al. 2006) |
7 0.5 |
5 min 1 min |
> 3 > 4 |
Feline calicivirus Human adenovirus type 1(SARS-CoV surrogate) Avian influenza virus Swine influenza virus |
| Sodium hypochlorite (Dellanno C et al. 2009; Cavalli A et al. 2018 ) |
0.21 0.75, 0.38 |
30s < 60s, > 15 min |
> 3 > 3 |
MHV (a potential surrogate for SARS-CoV) Canine parvo-virus-2 |
| Phenol (Weber DJ et al. 1999) | 0.5 | 30 | - | HIV, HSV, hepatitis B, and enveloped viruses |
| Quaternary compound (Belliot et al. 2008; Girard et al. 2010; Whitehead and McCue 2010) | < 3 | MNV and FCV titers | ||
| Quaternary compound and ethanol (Dellanno C et al. 2009) glutaraldehyde, QAC and isopropanol (W Zonta et al. 2016) |
0.10 + 79 | 30 | > 3 > 3 |
MHV (a potential surrogate for SARS-CoV) MNV and FCV titers |
Combination 1: applying 61% of Ethanol and 1% Chlorohexidine combination had a significant increase in log10 value in bacterial CFU reduction [12]. Combination 2:78% alcohol with Povidine-Iodine (3.2%) demonstrated excellent virucidal efficacy against the Ebola virus even at 15-second of application in-vitro experiments [13]. Combination 3: ethanol 69.39% w/w,2-propanol 3.69 % w/w, citric acid 2%and urea 2% was found capable of inactivating all enveloped and non-enveloped viruses at an exposure time of the 60S [14].
Iodine + Povidine: Povidine-iodine (PVP-I) comes under broad-spectrum antimicrobial agents. PVP-I has well known general antimicrobial activity, especially when considering resistant organisms [15]. Recent studies reported the use of 7.5% of PVP-I as a hand washing agent which significantly reduced enveloped virus load by 5 log10 reduction factor within 15 s [15,16]. In contrast to this, a case study evidenced respiratory distress due to aspiration of Povidine- iodine solution [17].
Chlorohexidine: Chlorohexidine is used as standard and conventional perioperative hand sanitizers alone and in combination with alcohol [13,18]. However, it is effective against bacteria like E. coli by reducing the colony-forming unit (CFU) by 4 log10 whereas it is effective against the enveloped virus but is not significantly reliable [16].
Soap and scrubs: Soaps are salts of fatty acid and potassium hydroxide (KOH). It has amphoteric properties and acts as a surfactant. Amphoteric properties involved in the inactivation of the virus by dissolving its lipid layer. Composition of Potassium oleate (C18:1), sodium laureth sulfate (LES) and sodium lauryl sulfate (SDS) has been reported to inactivate the enveloped virus (Influenza) [18]. Viral structure inactivation potential of potassium oleate soap is dependent on the positive surface charge present on the virus lipid layer [18]. Povidine iodine-based soap/surgical scrubs have significantly reduced viral load marginally as compared to normal soap [15].
The surface disinfectant used in house and hospital for cleaning purposes
Hydrogen peroxide: Hydrogen peroxide is considered to be a highly potent oxidizing agent that commonly acts against a wide range of micro-organisms including viruses and spore-forming organisms [19]. Hydroxyl-free radicals are a highly reactive product of hydrogen peroxide (H2O2), which plays a vital role in altering the associated proteins, lipids, and nucleic acid of viruses and bacteria and consequently inhibition of the infection and replication process of the viruses [20]. Micro-biocide action of 7% hydrogen peroxide has been shown to be effective against spores (6 hrs.), mycobacteria (20 minutes), fungi (5 minutes), viruses (5 minutes) and bacteria (3 minutes) at 1:16 dilution by using a quantitative carrier test [21,22]. A 0.5% accelerated hydrogen peroxide has been shown to have antibacterial and antiviral activity in 1 minute & anti-mycobacterial and anti-fungal activity in 5 minutes [21].
Phenol: Independent studies have demonstrated that phenolic compound has a potential effect against bacteria, fungi, and Viruses [22-25]. A 0.5% phenolic solution (2.7% ortho-benzyl-para-chlorophenol and 2.8% ortho-phenylphenol) denatured HIV and a 2% phenolic solution (6.3% para-tertiary-amyl phenol and 15% ortho-phenylphenol) denatured both enveloped and non-enveloped viruses [26]. Environmental surfaces exposed to sample (without visible blood) of infected individuals with HIV, HSV, or hepatitis B viruses can be disinfected with a 0.5% or 0.05% diluted phenolic solution [24]. But in the presence of blood, only 0.5% phenolic solution is effective. Furthermore, findings of the same studies have significantly differed across laboratories testing similar items.
Sodium hypochlorite: Generally, 0.5% of sodium hypochlorite solutions have been used as a disinfectant on inanimate surfaces, for water, fruit and vegetable purposes. It has a wide range of antimicrobials activities, leaves no toxic products, is water-resistant, inexpensive and readily available, and eliminates dry or fixed pathogens and biofilms from walls and floors [27,28]. Sodium hypochlorite solution (0.23%) shows potential against murine hepatitis virus (a potential surrogate for SARS coronavirus) in 30 seconds [29]. Sodium hypochlorite solution (0.75%) can significantly inactivate the canine parvovirus type 2 titers in 1 min but at lower concentration (0.37%) shows potential virucidal activity within 15 min [30].
Quaternary Ammonium Compounds (QAC): The quaternary ammonium (Didecyldimethyl-ammonium chloride) complexes are frequently used as disinfectants. Quaternary ammonium compounds used to disinfect materials or appliances for patients, including cystoscopes or cardiac catheters [31-33]. The quaternary antimicrobial activity has been directly related to the inactivation of enzymes generating energy, denaturation of integral cell proteins, and degradation of the cell membrane [34], 0.10% of the quaternary compound with 79% ethanol shows activity against MHV (SARS-CoV surrogate) with a log decrease > 3 log10 [30]. Glutaraldehyde reduced MNV and FCV titers significantly by > 6 log10 at a concentration of 2% [35], whereas MNV and FCV titers were reduced by < 3 log10 after QAC usage [35-37]. Glutaraldehyde, QAC, and isopropanol were shown to have a considerable effect on MNV and FCV surrogates with a log reduction of > 3 log10 [38]. Therefore, interactions between different substances are likely to occur and must be considered, e.g. having synergistic or antagonistic effects.
How to disinfect the common thing?
How to wash/clean the raw food/fruit?: Food hygiene and handling are of utmost importance at this time of pandemic. Many people use procedures like washing fruits and vegetables using soap or detergents prior to consuming it. There is still no evidence suggesting that Coronavirus can spread through food products or not. However, we must follow certain steps and common instructions to keep the food healthy and free from germs. Most government organizations advise simply washing the vagetables with fresh water, scrubbing it with a brush when required. We should not forget to have vegetable brush cleaned and dried between uses. Moreover, the sanitation of the preparation area and the equipment from sinks to cutting panels is equally significant [39].
The Washington State Department of Health and FDA recommend these guidelines for food staff and rest of us [40].
• The Washington State Department of Health and FDA recommend these guidelWho have coughing, feverishness, shortness of breath, vomiting or diarrhea or other signs of disease must stay out of the kitchen
• Hands should be washed pre and post preparation of the meal to minimize disease risk
• The raw agricultural products, such as lettuce heads should be washed properly under running water before being cut or served
Cooking for 30 minutes at 140 degrees Fahrenheit kills SARS according to the Food Safety Authority of Ireland [41]
How to use laundering in SARS pandemic?: In this current pandemic, wearing clothes is one of the carriers for SARS. In order to control this; safety in laundry process could play vital role. It has been reported that washing of cloths should be done at high temperatures like 71 °C for about 3 minutes or 65 °C for about 10 (“Guidelines for Environmental Infection Control in Health-Care Facilities: (545922006-001) [42] or Cold temperature wash: 20 °C with bleach (60-150 parts per million (ppm) available chlorine) (“Guidelines for Environmental Infection Control in Health-Care Facilities: (545922006-001) [42] or Ozone washing is a fairly new process for the 32 °C to 35 °C ambient washing cycle [43].
How to prevent the spreading of virus in lift?: SARS-CoV-2 may have transmitted rapidly through fomites (e.g. lifts or bathroom taps) or aerosol virus spray in public spaces in closed environments (e.g., toilets or lifts) [43]. In order to control the contamination following measures could be implemented such as Wipe lift and escalators, especially call buttons and stairs with detergent and water, or alternatively, disinfect it with 1 in 99 diluted domestic bleach solutions (5.25%), where applicable and regularly clean air vans for lifting.
Some important guidelines issued by the lift manufacturer could be practice to avoid the contamination.
DO-
• Practice social distancing in lifClean your hands and use disinfectant alcohol after touching of elevator buttons or staircases
• Avoid overcrowding
• Refrain from talking
• Do not lean on walls
How to disinfect the general facilities for fitness/sports complex?: In this pandemic, we have critical challenges for the perpetuation or return of physical activity and competition sports event. Moreover, we need to think about restarting the normal life, to overcome from the spreading of infection, we should practice the common hygiene and follow some strict guidelines such as; Public fitness areas and facilities should be cleaned using a 1 in 99 diluted household bleach solution (5.25%) and swept at least once every day. Satisfactory disinfectants (for example 70% alcohol) and paper towels are to be made frequently accessible to users and workers in the fitness center/sports complex in order to encourage regular cleaning. All clothes issued by gymnasium or health club must be washed using lukewarm water (70°C - 80 °C) cycle (“Guidelines for Environmental Infection Control in Health-Care Facilities: (545922006-001) [42].
How to sanitize the hospital/mask/paper/conference hall?: The COVID-19 pandemic continues, and on the other hand healthcare facilities are limited of masks, gowns as well as other personal protective equipment (PPE). UV light, could be used for disinfecting hospital rooms, operating centers, mask, official paper as well as conference halls, is one approach to do so [44]. UV therapy will be a step in a multi-barrier approach. This means using it in combination with other methods for disinfection, such as treatment with hydrogen peroxide. This will lessen the chances of infection. Vacuum UV light provides an effective solution against various environmental and pathogenic micro-organisms like E. coli, Staphylococcus aureus resistant to methicillin, and seasonal influenza viruses [45].
The clinical evidence on the percentage yield of various disinfectants against SARS-COV-2 is limited. This systemic review compares the existing hand sanitizers and surface disinfectants for different enveloped and non-enveloped viruses and optimized the best hand sanitizers and surface disinfectants for SARS-CoV 19. Generally, Soap and ethanol have been used as a broad spectrum Antiviral and antibacterial hand sanitizers [18,43]. Ethanol-based hand sanitizers have immediate and effective action against several enveloped viruses including orthopoxvirus, influenza a virus, SARS CoV, MERS CoV, HSV type 1, Newcastle disease virus, HBV and HIV [46]. An Infected individual with SARS-COV-2 is supremely contagious and is most likely to contaminate proximal inanimate surfaces or nearby surroundings. SARS CoV 2 may persist on inanimate surfaces for 9 days at room temperature and this survival rate makes this strain distinctively contagious [22]. Although limited shreds of evidence are available on spreading of SARS-COV-2 from a contaminated surface to hands, it is suggested that Influenza A virus can transfer 31.6% of the viral load to the hand within 5 s [29]. It is reported from statistical data, that humans touch their face with own hands at least 23 times per hour. Briefly, humans mostly contact the skin by hand (56%), followed by mouth (36%), nose (31%) and eyes (31%). In order to control the spreading of the deadly virus, disinfectant plays a major role including hand sanitizers and surface disinfectants [24]. Ethanol is the major ingredient of the hand sanitizers against enveloped virus including SARS CoV. Studies showed, 80% of ethanol is effective against most of the enveloped and non-enveloped viruses [11]. However, 85% of ethanol has shown a similar reduction factor against SARS-CoV (5.5 log10) as compared to 95% ethanol [10,11]. In addition, ethanol can be effective against enveloped virus at lower concentrations with other virucidal agents [12,14,47,48]. Combination 2 and combination 3 are significantly effective (log10 > 4) against enveloped virus and non-enveloped virus in comparison to combination 1 including presented ethanol combinatorial agent [13]. Povidone-Iodine (PVP-I), Chlorohexidine, and soap are other alternatives to be used as hand sanitizers against enveloped viruses and non-enveloped viruses [12,13,18]. PVP-I: 7.5% of PVP-I effective against enveloped [13] however, standard care and protection are the necessary elements during application of PVP-I are exclusively in respiratory disorders [17]; Chlorohexidine: 4% of Chlorohexidine is reported to be effective against bacteria like E. coli by reducing the colony-forming unit (CFU) by 4 log10 [46]; Soap: soaps have distinct amphoteric nature which helps to dissolve the lipid bilayer membrane of enveloped viruses including SARS-CoV [18]. In comparison to surface disinfectant, sodium hypochlorite or a mixture of glutaraldehyde, QAC and isopropanol shows the highest reduction with 3 log10 at a lower concentration. For further advancement and current pandemic scenario, it is interesting to look towards accelerated hydrogen peroxide as an active ingredient of the quick surface disinfectant automated machine ( tunnel system) as this ingredient shows effective against enveloped viruses and non-enveloped viruses including Human adenovirus type 1(SARS-CoV surrogate) at lower concentration of 0.5% within 60 seconds.
Our comparative studies concluded that 85% ethanol-based sanitizers and Povidine iodine-based soap/surgical scrub could be preferred hand sanitizers against enveloped viruses including SARS-CoV2. For surface eradication, 0.5% sodium hypochlorite or a mixture of glutaraldehyde, QAC, and isopropanol could have more efficacies as compared to hydrogen peroxide, phenol, and QAC alone. Accelerated hydrogen peroxide, an active component in the automatic surface disinfectant machine (tunnel system) for the pandemic situation, could be a positive indication for quick whole body sanitation. In addition, following certain strict guidelines issued by healthcare and government agencies, a normal life may be resumed.
Declarations
Authors’ contributions: The concept was conceived by AR as well as writing of the manuscript was done by him. Data collection and screening was done by SP. NS and HS have contributed equally in writing ad screening of article. PS, AP and BM were contacted for final review of the manuscript.
- A TP. The Classification of Viruses. Annu Rev Microbiol. 1996.
- Weissenhorn W, Dessen A, Calder LJ, Harrison SC, Skehel JJ, et al. Structural basis for membrane fusion by enveloped viruses. Mole Membr Biol. 1999; 16: 3-9. PubMed: https://pubmed.ncbi.nlm.nih.gov/10332732/
- Cromeans TL, Kahler AM, Hill VR. Inactivation of Adenoviruses, Enteroviruses, and Murine Norovirus in Water by Free Chlorine and Monochloramine. Appl Environ Microbiol. 2010; 76: 1028-1033. PubMed: https://pubmed.ncbi.nlm.nih.gov/20023080/
- MP. Modes of action of disinfectants. 1995.
- Sharp DG, Leong J. Inactivation of poliovirus I (Brunhilde) single particles by chlorine in water. Appl Environ Microbiol. 1980; 40: 381–385. PubMed: https://pubmed.ncbi.nlm.nih.gov/6258476/
- Thurman RB, Gerba CP. Molecular Mechanisms of Viral Inactivation by Water Disinfectants. Adv Appl Microbiol. 1985; 75–105. https://linkinghub.elsevier.com/retrieve/pii/S0065216408702053
- Al-Qahtani AA. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): Emergence, history, basic and clinical aspects. Saudi J Biol Sci. 2020; 27: 2531–2538. PubMed: https://pubmed.ncbi.nlm.nih.gov/32336927/
- Chen X, Ran L, Liu Q, Hu Q, Du X, et al. Hand Hygiene, Mask-Wearing Behaviors and Its Associated Factors during the COVID-19 Epidemic: A Cross-Sectional Study among Primary School Students in Wuhan, China. Int J Environ Res Public Health. 2020; 17: 2893. PubMed: https://pubmed.ncbi.nlm.nih.gov/32331344/
- Walsh KA, Jordan K, Clyne B, Rohde D, Drummond L, et al. SARS-CoV-2 detection, viral load and infectivity over the course of an infection. J Infect. 2020; 81: 357–371. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7323671/
- Steinmann J, Becker B, Bischoff B, Magulski T, Steinmann J, et al. Virucidal activity of Formulation I of the World Health Organization’s alcohol-based handrubs: Impact of changes in key ingredient levels and test parameters. Antimicrob Resist Infect Control. 2013; 2. PubMed: https://pubmed.ncbi.nlm.nih.gov/24330802/
- Rabenau HF, Kampf G, Cinatl J, Doerr HW. Efficacy of various disinfectants against SARS coronavirus. J Hospital Infect. 2005; 61: 107-111. PubMed: https://pubmed.ncbi.nlm.nih.gov/15923059/
- Eggers M, Koburger-Janssen T, Ward LS, Newby C, Müller S. Bactericidal and Virucidal Activity of Povidone-Iodine and Chlorhexidine Gluconate Cleansers in an In Vivo Hand Hygiene Clinical Simulation Study. Infect Dis Ther. 2018; 7: 235-247. PubMed: https://pubmed.ncbi.nlm.nih.gov/29761329/
- Eggers M, Eickmann M, Kowalski K, Zorn J, Reimer K. Povidone-iodine hand wash and hand rub products demonstrated excellent in vitro virucidal efficacy against Ebola virus and modified vaccinia virus Ankara, the new European test virus for enveloped viruses. BMC Infect Dis. 2015; 15: 375. PubMed: https://pubmed.ncbi.nlm.nih.gov/26381737/
- Ionidis G, Hübscher J, Jack T, Becker B, Bischoff B, et al. Development and virucidal activity of a novel alcohol-based hand disinfectant supplemented with urea and citric acid. BMC Infect Dis. 2016: 16: 77 PubMed: https://pubmed.ncbi.nlm.nih.gov/26864562/
- Sauerbrei A, Wutzler P. Virucidal efficacy of povidone-iodine-containing disinfectants: Virucidal efficacy of PVP-iodine. Lett Appl Microbiol. 2010.
- Tsai JC, Lin YK, Huang YJ, Loh EW, Wen HY, et al. Antiseptic Effect of Conventional Povidone–Iodine Scrub, Chlorhexidine Scrub, and Waterless Hand Rub in a Surgical Room: A Randomized Controlled Trial. Infect Control Hosp Epidemiol. 2017; 38: 417-422 PubMed: https://pubmed.ncbi.nlm.nih.gov/27995837/
- Hitosugi T, Tsukamoto M, Yokoyama T. Pneumonia due to aspiration of povidine iodine after preoperative disinfection of the oral cavity. Oral Maxillofac Surg. 2019; 23: 507-511. PubMed: https://pubmed.ncbi.nlm.nih.gov/31673818/
- Kawahara T, Akiba I, Sakou M, Sakaguchi T, Taniguchi H. Inactivation of human and avian influenza viruses by potassium oleate of natural soap component through exothermic interaction. In T. Webster (Ed.), PLoS ONE. 2018.
- Cords BR, Sanitizers DGR. Halogens, surface-active agents and peroxides: Antimicrobials in foods. PM and Branen, AL. Marcel Dekker Inc. 1993.
- McDonnell G, Russell AD. Antiseptics and disinfectants: Activity, action, and resistance. Clinical Microbiology Rev. 1999; 12: 147–179. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC88911/
- Omidbakhsh N, Sattar SA. Broad-spectrum microbicidal activity, toxicologic assessment, and materials compatibility of a new generation of accelerated hydrogen peroxide-based environmental surface disinfectant. Am J Infect Control. 2006; 34: 251–257. PubMed: https://pubmed.ncbi.nlm.nih.gov/16765201/
- Sattar SA, Springthorpe VS. Survival and disinfectant inactivation of the human immunodeficiency virus: A critical review. Reviews of Infectious Diseases. 1991.
- Bird CE, Criqui MH, Fronek A, Denenberg JO, Klauber MR, et al. Quantitative and qualitative progression of peripheral arterial disease by non-invasive testing. Vasc Med. 1999; 4: 15–21.
- Rutala WA, Weber DJ. 2004.
- Spaulding EH. Chemical disinfect of medical and surgical materials. Disinfection, sterilization and preservation. 1968.
- Weber DJ, Barbee SL, Sobsey MD, Rutala WA. The effect of blood on the antiviral activity of sodium hypochlorite, a phenolic, and a quaternary ammonium compound. Inf Control Hospital Epidemiol. 1999; 20: 821–827. PubMed: https://pubmed.ncbi.nlm.nih.gov/10614606/
- Jakobsson SW, Rajs J, Jonsson JA, Persson H. Poisoning with sodium hypochlorite solution. Report of a fatal case, supplemented with an experimental and clinico-epidemiological study. Am J Foren Med Pathol. 1991; 12: 320-327. PubMed: https://pubmed.ncbi.nlm.nih.gov/1807142/
- Merritt K, Hitchins VM, Brown SA. Safety and cleaning of medical materials and devices. Journal of Biomedical Materials Research: An Official Journal of The Society for Biomaterials, The Japanese Society for Biomaterials, and The Australian Society for Biomaterials and the Korean Society for Biomaterials. 2000; 53: 131–136.
- Dellanno C, Vega Q, Boesenberg D. The antiviral action of common household disinfectants and antiseptics against murine hepatitis virus, a potential surrogate for SARS coronavirus. Am J Infect Control. 2009; 37: 649–652. PubMed: https://pubmed.ncbi.nlm.nih.gov/19692148/
- Cavalli A, Marinaro M, Desario C, Corrente M, Camero M, et al. In vitro virucidal activity of sodium hypochlorite against canine parvovirus type 2. Epidemiol Infect. 2018; 146: 2010–2013. PubMed: https://pubmed.ncbi.nlm.nih.gov/30178730/
- Ehrenkranz NJ, Bolyard E, Wiener M, Cleary T. Antibiotic-sensitive Serratia marcescens infections complicating cardiopulmonary operations: Contaminated disinfectant as a reservoir. Lancet. 1980; 316; 1289–1292.
- Sehulster LM. Healthcare laundry and textiles in the United States: Review and commentary on contemporary infection prevention issues. Infect Control Hospital Epidemiol. 2020.
- Shickman MD, Guze LB, Pearce ML, Yamashita J. Bacteremia following cardiac catheterization: Report of a case and studies on the source. New Engl J Med. 1959; 260: 1164–1166.
- Shere L. Some comparisons of the disinfecting properties of hypochlorites and quaternary ammonium compounds. Milk Plant Monthly. 1948; 37: 66–69.
- D’Souza DH, Su X. Efficacy of chemical treatments against murine norovirus, feline calicivirus, and MS2 bacteriophage. Foodborne Pathogens is. 2010; 7: 319–326. PubMed: https://pubmed.ncbi.nlm.nih.gov/19919284/
- Belliot G, Lavaux A, Souihel D, Agnello D, Pothier P. Use of murine norovirus as a surrogate to evaluate resistance of human norovirus to disinfectants. Appl Environ Microbiol. 2008; 74: 3315–3318. PubMed: https://pubmed.ncbi.nlm.nih.gov/18378650/
- Whitehead K, McCue KA. Virucidal efficacy of disinfectant actives against feline calicivirus, a surrogate for norovirus, in a short contact time. Am J Infect Control. 2010; 38: 26–30. PubMed: https://pubmed.ncbi.nlm.nih.gov/19616346/
- Zonta W, Mauroy A, Farnir F, Thiry E. Comparative virucidal efficacy of seven disinfectants against murine norovirus and feline calicivirus, surrogates of human norovirus. Food Environ Virol. 2016; 8: 1-12. PubMed: https://pubmed.ncbi.nlm.nih.gov/26445948/
- Washington State Retail Food Code. (n.d.). 144.
- COVID-19 Information for Food Safety | Washington State Department of Agriculture. (n.d.). 2021. PubMed: https://agr.wa.gov/departments/food-safety/food-safety/covid-19-information-for-food-safety
- Coronavirus and Food Safety | FAQs | The Food Safety Authority of Ireland. (n.d.). 2021. https://www.fsai.ie/faq/coronavirus.html
- Guidelines for Environmental Infection Control in Health-Care Facilities: (545922006-001). Am Psychol Assoc. 2003.
- Century 21—Pregnant with Ozone: Ozone. (n.d.). Sci Engin. 24. https://www.tandfonline.com/doi/abs/10.1080/01919510208901590
- Cai J, Sun W, Huang J, Gamber M, Wu J, et al. Indirect Virus Transmission in Cluster of COVID-19 Cases, , Wenzhou, China, 2020. 2020; 26: 1343-1345. PubMed: https://pubmed.ncbi.nlm.nih.gov/32163030/
- Szeto W, Yam WC, Huang H, Leung DYC. The efficacy of vacuum-ultraviolet light disinfection of some common environmental pathogens. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7014767/
- Siddharta A, Pfaender S, Vielle NJ, Dijkman R, Friesland M, et al. Virucidal Activity of World Health Organization–Recommended Formulations Against Enveloped Viruses, Including Zika, Ebola, and Emerging Coronaviruses. J Infect Dis. 2017; 215: 902-906. PubMed: https://pubmed.ncbi.nlm.nih.gov/28453839/
- Biermann NM, McClure JT, Sanchez J, Saab M, Doyle AJ. Prospective, randomised clinical trial of four different presurgical hand antiseptic techniques in equine surgery. Equine Vet J. 2019; 51: 600-605. PubMed: https://pubmed.ncbi.nlm.nih.gov/30565715/
- Deshpande A, Fox J, Wong KK, Cadnum JL, Sankar T, et al. Comparative Antimicrobial Efficacy of Two Hand Sanitizers in Intensive Care Units Common Areas: A Randomized, Controlled Trial. Infect Control Hosp Epidemiol. 2018; 39: 267-271. PubMed: https://pubmed.ncbi.nlm.nih.gov/29382400/